Focus Article: Designed to be sustainable: Excerpts from the 2nd JADECARE Policy board meeting and policy dialogue
The JADECARE Policy board was established in 2021 at the beginning of this Joint Action, bringing together representatives of sixteen National health authorities and other institutions. The Policy Board members were appointed by the regions implementing adaptations of the best practice models of JADECARE (Next Adopters). They were recognised as relevant in (i) bridging the gap between the local pilot implementation settings and their regional/national policy levels, (ii) providing support with the implementation process, and (iii) increasing the potential for sustainability of developed solutions in digitally-enabled integrated person-centred care. Thus, the Policy board has an important advisory role in JADECARE. Moreover, its individual members can have a visible impact in assuring sustainability of pilot practices.
As the JADECARE implementation phase was concluding, the task leaders of the work package “Integration in National policies and Sustainability“ of JADECARE organised the 2nd Policy board meeting held in two steps: On November 17th 2022 for presenting and discussing interim results, status, challenges and successes of the implementation process. Moreover, it focused on sustainability building in two case studies (Italy and Germany) and on opportunities to strengthen the Member States capacities in integrated care via EU mechanisms and programmes. The consecutive 2nd Policy dialogue was convened a week later on November 24th with the aim to define key principles and recommended steps for Next Adopters in developing their Sustainability strategies and Sustainability action plans during the post-implementation phase in 2023.
In the first step, the 2nd Policy board meeting was attended by 47 representatives of JADECARE partner organisations, DG SANTE (Directorate-General for Health and Food Safety), DG REFORM (Directorate-General for Structural Reform Support), HaDEA (European Health and Digital Executive Agency), and JADECARE Policy board members. The meeting started with introductory presentations from Kronikgune (Coordinator of JADECARE), AGENAS and NIJZ (Leaders of work package “Integration in National policies and Sustainability”), welcoming the participants and presenting key results of the current work in JADECARE, including status of the implementation process in JADECARE; challenges and success factors during the first PDSA(Plan-Do-Study-Act) cycle of the implementation phase; and sustainability planning process aimed at supporting the implementers to enhance the sustainability of their practices upon conclusion of the Joint Action. Afterwards, representatives from DG SANTE and DG REFORM presented EU mechanisms and instruments to support integrated care practices and their sustainability, including different projects under the 3rd Health Programme (SCIROCCO Exchange, VIGOUR, JADECARE); Recovery and Resilience Facility; Healthier Together – EU NCD Initiative; and TSI (Technical Support Instrument programme) flagship project “Towards person-centred integrated care”. In conclusion, the Commission’s expectations for JADECARE were presented, namely the successful implementation (transfer/ adaptation) of pilot practices; increased knowledge/ capacity in implementing integrated care and confidence in the value of integrated care; and to plant the seeds for national/regional plans to mainstream integrated care.
Sustainability-oriented implementation experiences were illustrated by case studies from: 1.) Italy with its initiative to link JADECARE practices to Italy’s National resilience and recovery plan aimed at reinforcing practice sustainability and digital transformation of the healthcare system; and 2.) German partners planning to use JADECARE results to develop evidence-based recommendations for actions to transform the German Healthcare system towards integrated digitally-enabled person centred care, being involved in JADECARE in supportive work packages rather than being involved in the Joint Action as an implementer.
These experiences show the EU-added value of JADECARE, providing a platform for exchanging opportunities, ideas and knowledge in the field of integrated care that can expand far beyond the scope of a particular pilot setting.
The meeting was concluded by a Tour de Table among Policy Board members: “Critical appraisal of the two presented case studies and key messages identified” to discuss the presented case studies and share different implementation experiences or possible next steps to support the process of achieving JADECARE objectives.
In the second step, one week later, the 2nd Policy dialogue was held with Policy board members focusing on identification of key principles and recommended steps in development of Sustainability strategies and Sustainability action plans by all Next Adopters. These strategic documents are important to plan for the years upon conclusion of JADECARE to assure the continuity and evolution of developed solutions.
Important points of the facilitated discussions during the policy dialogue are summarized below:
- Clarity of vision and translation into action: a vision and purpose of the practice should be clear and most importantly, a result of involvement of a broad spectrum of partners that are affected by or can support the practice. This also means that the practice leaders (or holders of sustainability) should understand what motivates and drives participating actors. The vision should be ‘broken down’ to clear, measurable goals and activities with realistic planning (where responsibilities, timelines, expected outcomes/indicators have been defined).
- Adaptiveness of (Sustainability) Action plans: contextual factors might influence the implementation of practices in a positive or negative way. Sometimes these same factors can have different impacts in different settings as is the case with COVID-19 pandemic. For example, in Estonia it resulted in under-resourced activities related to integrated care despite the fact it remains one of the key priorities at the national level. On the other hand, as is the case with Italy, the pandemic pushed the policy makers to make significant investments into digitalisation and integration of care. The experience suggests, the practice owners should be attentive and flexible to the changing environment and align their activities and plans according to the emerging needs and opportunities.
- Overcoming projectism: dependency on project resources can be an issue on the long run and can hamper the practice sustainability. This is why it is important to plan significantly in advance how the (systemic) funding and resources will be assured upon its conclusion. Consequently, the practices should be aligned to the larger scale of health system transformation, including policies, strategies and EU mechanisms and instruments to become embedded into the local health ecosystem. In this respect, support of political leadership is very much needed. On the other hand, projects such as JADECARE created strong networks across Member States and established valuable channels for knowledge exchange. Nurturing this collaboration also in the future can have significant impacts on integrated care initiatives across Europe and thus increases EU-added value of Joint Actions such as this one.
- Advocating for a co-creation approach: meaningful and continuous involvement of relevant stakeholders can be a demanding task. Next Adopters have been supported throughout this Joint Action to build multidisciplinary networks of partners from various professional organisations, healthcare organisations, local/regional/national health authorities. To varying degree, patient and citizen organisations have been included as well. Inclusion of target groups (patients, citizens, care providers) is especially important for the overall acceptance, adaptability and continuity of integrated care practices and should be considered also during sustainability planning process.
The inputs from the Policy board have meaningfully contributed to the development of a sustainability planning approach in JADECARE and have helped to be reflective in developing Sustainability strategies and Sustainability action plans of Next Adopters. We are now taking a look forward to the third (and final) Policy board meeting to be held on June 20, 2023, and policy dialogue on June 22, 2023, and towards the times beyond this Joint Action.…
Got newsletter forwarded? Click here for subscribing for your own copy
Focus Article: JADECARE insights in original Good Practice transfer: Effects of ‘Sports on Prescription’ on Patient Health and Wellbeing
Eurometropole de Strasbourg (EUSTRAS) is a partner in the JADECARE Joint Action that has chosen acting as a Next Adopter for the original Good Practice “The OptiMedis model – integrated population-based care (Germany)”. This model targets simultaneously better population health supported by population data analysis, an improved patient experience of care including increased service quality and higher patient satisfaction and reduced per capita costs of health care by increasing system efficiency. Inter alia, it embraces transforming regional health care delivery using a people centred approach to deliver care services and also leveraging health by preventive action and citizen activation. Within their JADECARE related activities, EUSTRAS and Optimedis colleagues (see list of authors* in paragraph “the present study ..”) have reported their results in an abstract submitted and accepted for the International Conference on Integrated Care (ICIC) 2022 in Odense, Denmark.

Effects of ‘Sports on Prescription’ on Patient Health and Wellbeing: The effects of physical activity programs for primary prevention and avoiding disease aggravation are well described. The French national healthcare strategy “Ma Santé 2022” calls for a more integrated and multi-sectoral health care delivery system at primary care level with a stronger focus on health promotion and primary and secondary prevention programs such as health education and physical activity programs. Through its Local Health Contracts (CLS), the city of Strasbourg has funded an opportunity for local physicians to prescribe the participation in physical activity programs to their patients since 2012 (i.e. Sport Santé sur Ordonnance (SSSO)). Eligible patients may directly, or after a clinical rehabilitation period, join a three-year physical activity program which includes individual monitoring (motivational counselling, physical activity measurements) and regular sport sessions (adapted physical activity in groups). At this stage, around 4000 individuals were included in these programs (mean age = 52 years old). However, concrete outcomes on patient satisfaction and wellbeing as well as on potential changes in health service consumption remain unclear.
The present analysis (joint abstract/presentation at ICIC 2022 by* François Jouan [Groupement d’Intérêt Public – Maison Sport Santé de Strasbourg (GIP-MSS), France], Colin Majean [Caisse Primaire d’Assurance Maladie (CPAM) du Bas Rhin, France], Caroline Schuster [Eurométropole de Strasbourg, France, Matthieu Jung [GIP-MSS], Pauline Blanc [GIP-MSS], Manfred Zahorka [OptiMedis AG, Hamburg, Germany]) was conducted in the framework of the JADECARE Joint Action and looks at patient outcomes in terms of functional status, wellbeing, and effects on the consumption of healthcare services from patients, who were included in the SSSO program between 01/01/2020 and 12/31/2021 (N= 864 (mean age=53.5 years old, Female 72%, Male 28%, 88% have at least one and 28% at least 2 chronic conditions).
Only routine data from the local health insurer and project data from the SSSO data base were used for this analysis. No primary data collection was done. A combination with patient satisfaction data was anticipated at the beginning but failed due to lack of repeated measurements. For the analysis of program effects on health care costs data from the participant database from the SSSO program were matched with data from the public health insurer (CPAM du Bas Rhin). Patient functional status was assessed at the beginning, during and at the end of the program. For health care services consumption, health insurance data from program participants were compared with matched non-participants. Matching was done on age, gender, residence, and diagnosis.
The analysis showed a clear improvement of patients’ functional status based on patient perception as well as on the physical assessment. Figure 1 shows the result of an exercise strengthening people’s balance to prevent falls. Participants were asked to stand on one leg and the maximum duration was measured (in seconds) at the beginning of the physical exercise program as well as in half year intervals from the start. The graphic shows a steady increase of people’s capacity over the training period amounting to a 50% longer duration at the end of the follow-up period.
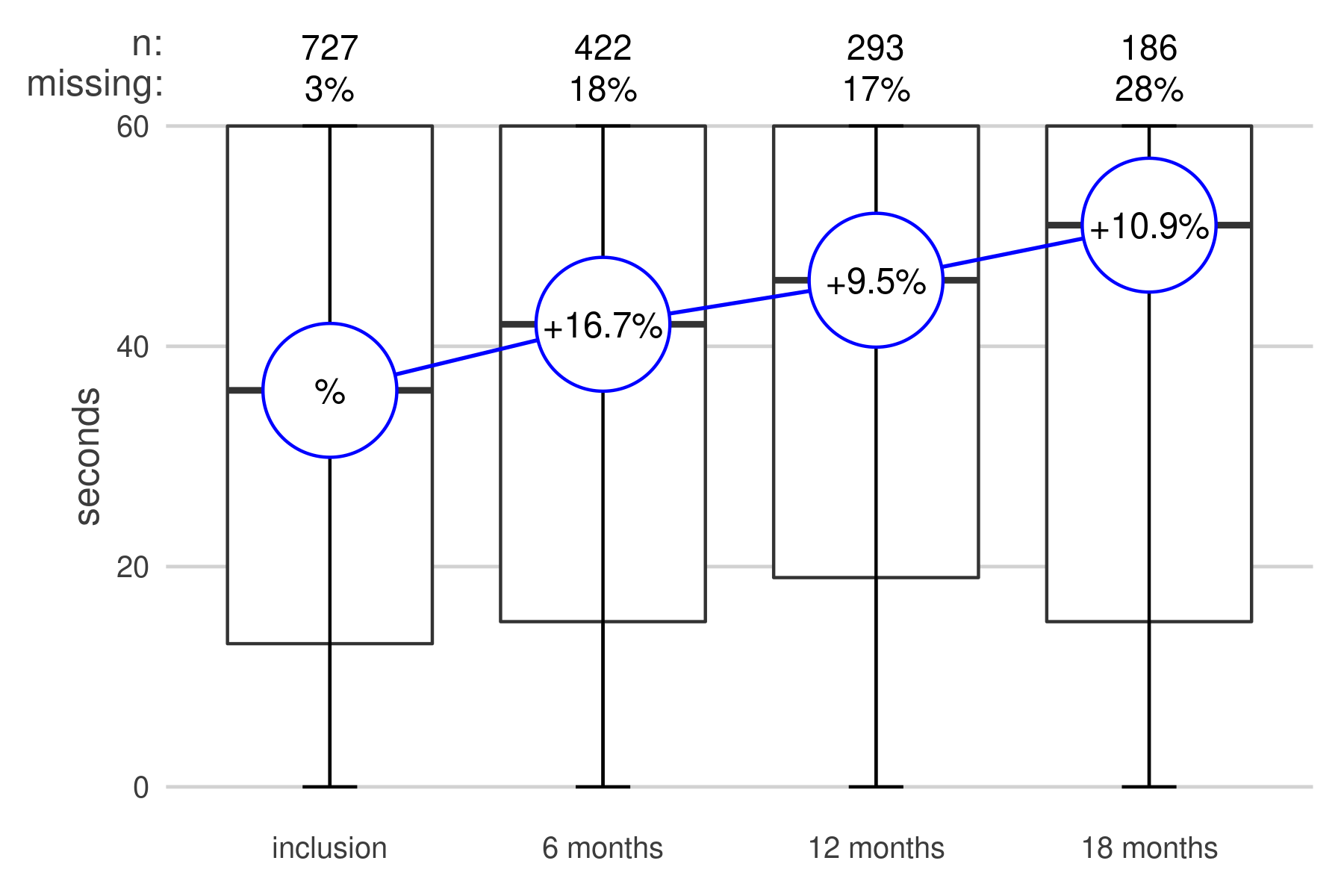
Figure 1: Improvements of physical balance (1 leg stand) over a period of 1.5 years.
Matching physical activity data with health services consumption data also showed an improvement in general well-being, expressed by a reduction in health care services consumption.
Only routine data from the local health insurer and project data from the SSSO data base were used for this analysis. No primary data collection was done. A combination with patient satisfaction data was anticipated at the beginning but failed due to lack of repeated measurements. For the analysis of program effects on health care costs data from the participant database from the SSSO program were matched with data from the public health insurer (CPAM du Bas Rhin). Patient functional status was assessed at the beginning, during and at the end of the program. For health care services consumption, health insurance data from program participants were compared with matched non-participants. Matching was done on age, gender, residence, and diagnosis.
The analysis showed a clear improvement of patients’ functional status based on patient perception as well as on the physical assessment. Figure 1 shows the result of an exercise strengthening people’s balance to prevent falls. Participants were asked to stand on one leg and the maximum duration was measured at the beginning of the physical exercise program as well as in half year intervals from the start. The graphic shows a steady increase of people’s capacity over the training period amounting to a 50% longer duration at the end of the follow-up period. Matching physical activity data with health services consumption data also showed an improvement in general well-being, expressed by a reduction in health care services consumption.
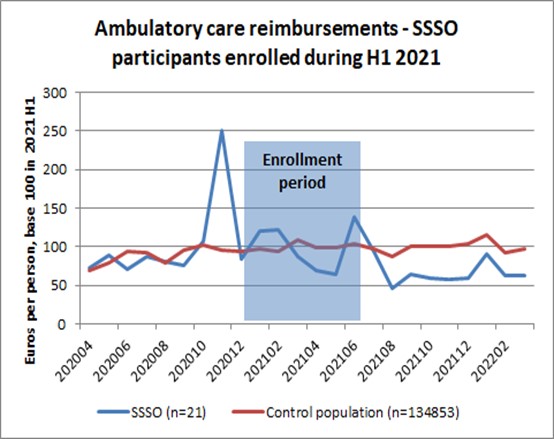
Figure 2 (Ambulatory care reimbursements for participants of SSSO following enrolment in physical exercise courses compared to standard population) shows changes in health care consumption trends of a group of participants in SSSO programs following their inscription in the training programs (blue line). The development is compared with a standard population of the same geographic area (red line). Health care consumption of the sports on prescription group (SSSO) is generally higher than for the standard population. For the comparison of trends, the values for both groups were normalised. The analysis of health insurance data showed some effects on health care costs, mostly in terms of the number of doctors’ visits and drug utilisation compared to non-users of SSSO services. The mean reimbursement trends show strong differences in absolute values between SSSO group and controls. The SSSO group shows a 35% downward trend following the enrolment period whereas the trend for the control is a 12% upward trend. Due to the availability of health insurance data for two years only, the effects can however not be shown over the entire patient intervention period (3 years). Patient satisfaction was not repeatedly assessed so that no conclusions can be drawn on possible improvement trends at this stage.
A limitation of this study is the short surveillance time as well as a relatively small sample size for the SSSO group, which limits the quality of the matching process as well as the possibility of subgroup analysis.
Assessing concrete patient outcomes of interventions offers a new way of looking at the effectiveness and efficiency of health care interventions. The current study suggests that mobilising patients and people at risk for physical activity programs may improve patient’s functional status and general wellbeing as shown by their utilisation patterns of medical services.
It also shows that routine data can be used to show trends and effects of prevention programs on people’s health. Longitudinal patient data linked to concrete interventions is not readily available and requires inter-linking of several databases.
The present study used quite simple methods of matching users and non-users of SSSO services so that the significance of drawn conclusions might be limited.
Got newsletter forwarded? Click here for subscribing for your own copy
JADECARE Newsletter Subscription:
Load content below to proceed
Click on the button to load the content from 8f23b36d.sibforms.com.