Eurometropole de Strasbourg (EUSTRAS) is a partner in the JADECARE Joint Action that has chosen acting as a Next Adopter for the original Good Practice “The OptiMedis model – integrated population-based care (Germany)”. This model targets simultaneously better population health supported by population data analysis, an improved patient experience of care including increased service quality and higher patient satisfaction and reduced per capita costs of health care by increasing system efficiency. Inter alia, it embraces transforming regional health care delivery using a people centred approach to deliver care services and also leveraging health by preventive action and citizen activation. Within their JADECARE related activities, EUSTRAS and Optimedis colleagues (see list of authors* in paragraph “the present study ..”) have reported their results in an abstract submitted and accepted for the International Conference on Integrated Care (ICIC) 2022 in Odense, Denmark.
This article covers the content and illustrations presented at the conference:
The effects of physical activity programs for primary prevention and avoiding disease aggravation is well described. The French national healthcare strategy “Ma Santé 2022” calls for a more integrated and multi-sectoral health care delivery system at primary care level with a stronger focus on health promotion and primary and secondary prevention programs such as health education and physical activity programs.
Through its Local Health Contracts (CLS), the city of Strasbourg has funded an opportunity for local physicians to prescribe the participation in physical activity programs to their patients since 2012 (i.e. Sport Santé sur Ordonnance (SSSO)). Eligible patients may directly, or after a clinical rehabilitation period, join a three-year physical activity program which includes individual monitoring (motivational counselling, physical activity measurements) and regular sport sessions (adapted physical activity in groups). At this stage, around 4000 individuals were included in these programs (mean age = 52 years old). However, concrete outcomes on patient satisfaction and wellbeing as well as on potential changes in health service consumption remain unclear.
The present analysis (joint abstract/presentation at ICIC 2022 by* François Jouan [Groupement d’Intérêt Public – Maison Sport Santé de Strasbourg (GIP-MSS), France], Colin Majean [Caisse Primaire d’Assurance Maladie (CPAM) du Bas Rhin, France], Caroline Schuster [Eurométropole de Strasbourg, France, Matthieu Jung [GIP-MSS], Pauline Blanc [GIP-MSS], Manfred Zahorka [OptiMedis AG, Hamburg, Germany]) was conducted in the framework of the JADECARE Joint Action and looks at patient outcomes in terms of functional status, wellbeing, and effects on the consumption of healthcare services from patients, who were included in the SSSO program between 01/01/2020 and 12/31/2021 (N= 864 (mean age=53.5 years old, Female 72%, Male 28%, 88% have at least one and 28% at least 2 chronic conditions).
Only routine data from the local health insurer and project data from the SSSO data base were used for this analysis. No primary data collection was done. A combination with patient satisfaction data was anticipated at the beginning but failed due to lack of repeated measurements. For the analysis of program effects on health care costs data from the participant database from the SSSO program were matched with data from the public health insurer (CPAM du Bas Rhin). Patient functional status was assessed at the beginning, during and at the end of the program. For health care services consumption, health insurance data from program participants were compared with matched non-participants. Matching was done on age, gender, residence, and diagnosis.
The analysis showed a clear improvement of patients’ functional status based on patient perception as well as on the physical assessment. Figure 1 shows the result of an exercise strengthening people’s balance to prevent falls. Participants were asked to stand on one leg and the maximum duration was measured (in seconds) at the beginning of the physical exercise program as well as in half year intervals from the start. The graphic shows a steady increase of people’s capacity over the training period amounting to a 50% longer duration at the end of the follow-up period.
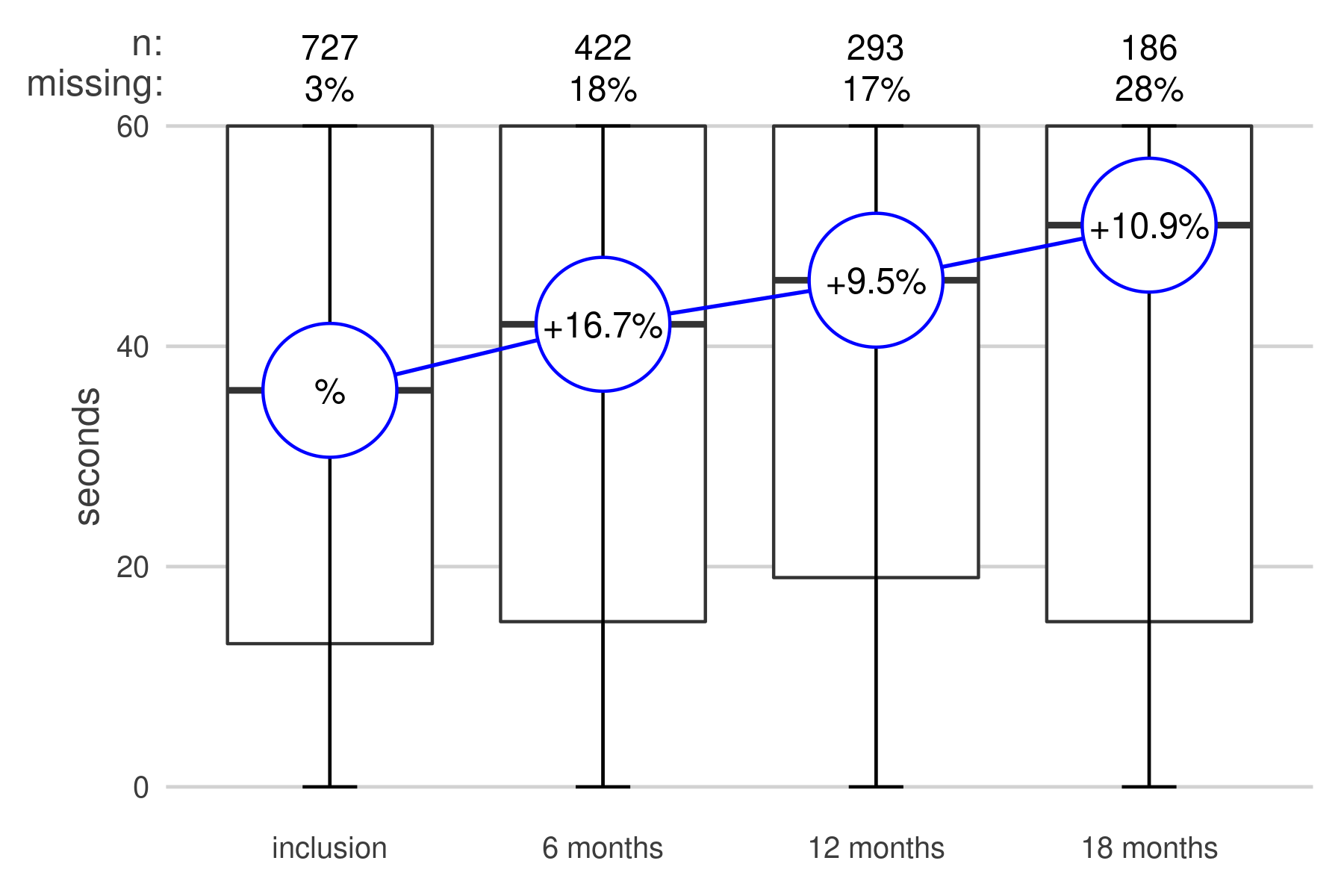
Figure 1: Improvements of physical balance (1 leg stand) over a period of 1.5 years.
Matching physical activity data with health services consumption data also showed an improvement in general well-being, expressed by a reduction in health care services consumption.
Only routine data from the local health insurer and project data from the SSSO data base were used for this analysis. No primary data collection was done. A combination with patient satisfaction data was anticipated at the beginning but failed due to lack of repeated measurements. For the analysis of program effects on health care costs data from the participant database from the SSSO program were matched with data from the public health insurer (CPAM du Bas Rhin). Patient functional status was assessed at the beginning, during and at the end of the program. For health care services consumption, health insurance data from program participants were compared with matched non-participants. Matching was done on age, gender, residence, and diagnosis.
The analysis showed a clear improvement of patients’ functional status based on patient perception as well as on the physical assessment. Figure 1 shows the result of an exercise strengthening people’s balance to prevent falls. Participants were asked to stand on one leg and the maximum duration was measured at the beginning of the physical exercise program as well as in half year intervals from the start. The graphic shows a steady increase of people’s capacity over the training period amounting to a 50% longer duration at the end of the follow-up period. Matching physical activity data with health services consumption data also showed an improvement in general well-being, expressed by a reduction in health care services consumption.
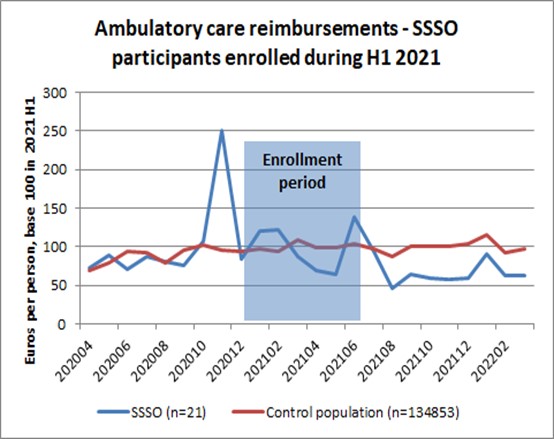
Figure 2 (Ambulatory care reimbursements for participants of SSSO following enrolment in physical exercise courses compared to standard population) shows changes in health care consumption trends of a group of participants in SSSO programs following their inscription in the training programs (blue line). The development is compared with a standard population of the same geographic area (red line). Health care consumption of the sports on prescription group (SSSO) is generally higher than for the standard population. For the comparison of trends, the values for both groups were normalised. The analysis of health insurance data showed some effects on health care costs, mostly in terms of the number of doctors’ visits and drug utilisation compared to non-users of SSSO services. The mean reimbursement trends show strong differences in absolute values between SSSO group and controls. The SSSO group shows a 35% downward trend following the enrolment period whereas the trend for the control is a 12% upward trend. Due to the availability of health insurance data for two years only, the effects can however not be shown over the entire patient intervention period (3 years). Patient satisfaction was not repeatedly assessed so that no conclusions can be drawn on possible improvement trends at this stage.
A limitation of this study is the short surveillance time as well as a relatively small sample size for the SSSO group, which limits the quality of the matching process as well as the possibility of subgroup analysis.
Assessing concrete patient outcomes of interventions offers a new way of looking at the effectiveness and efficiency of health care interventions. The current study suggests that mobilising patients and people at risk for physical activity programs may improve patient’s functional status and general wellbeing as shown by their utilisation patterns of medical services.
It also shows that routine data can be used to show trends and effects of prevention programs on people’s health. Longitudinal patient data linked to concrete interventions is not readily available and requires inter-linking of several databases.
The present study used quite simple methods of matching users and non-users of SSSO services so that the significance of drawn conclusions might be limited.
